원위부 담관암의 폐전이로 의심된 COVID-19 감염 후 발생한 폐크립토콕쿠스증
Pulmonary Cryptococcosis Mimicking Metastasis in a Distal Common Bile Duct Cancer Patient after Recent COVID-19 Infection
Article information
Abstract
담관암의 유일한 치료 방법은 수술로, 수술 가능성 평가가 진단 과정에 있어 매우 중요하다. 처음 진단 당시에는 원격 전이가 확인되지 않아 수술적 치료를 계획하던 중 다발성의 폐결절이 새롭게 확인되었던 원위부 총담관암 증례를 문헌고찰과 함께 보고한다. 원발 부위의 원위부 총담관암의 크기 변화는 없어 폐 전이 외의 감별진단이 필요하다고 판단하였다. 최근 COVID-19 감염력이 있던 증례로 수술 생검 결과상 최종적으로 폐 크립토코코스증으로 진단되었다.
Trans Abstract
The only curative treatment option for cholangiocarcinoma is surgery, making the assessment of operability a crucial step in the diagnosis. We report a case of distal common bile duct cancer in a 64-year-old male, who exhibited multiple pulmonary nodules in pre-operative chest imaging following a COVID-19 infection. As the local progression of disease was not prominent, the possibility of pulmonary metastasis was considered unlikely. A surgical biopsy was performed, which confirmed the diagnosis of pulmonary cryptococcosis.
INTRODUCTION
Cholangiocarcinoma is a malignant tumor originating from the epithelium of the bile duct [1]. The incidence of cholangiocarcinoma is higher in parts of the Eastern world compared to the west [2]. According to data from the National Cancer Information Center of Korea, biliary tract cancers ranked ninth, compromising 2.7% of all new cancer cases in 2021. The age-adjusted incidence rate per 100,000 population was 14.8 during the observation period. The incidence of biliary tract cancers is not decreasing, emphasizing the need for national attention and response [3]. Complete tumor resection remains the sole curative option for cholangiocarcinoma. The median overall survival is 21.9 months for resected patients, 6.7 months for unresected non-metastatic patients, and 3.6 months for metastatic patients, highlighting significant differences in survival outcomes according to resectability [4]. Therefore, accurately staging the tumor preoperatively and choosing the appropriate treatment through multidisciplinary approach are crucial for determining proper treatment [5,6].
Cholangiocarcinoma primarily spreads to surrounding structures including vessels, lymph nodes or liver parenchyma adjacent to the bile duct. Distant metastases can occur later in the disease course, most commonly affecting the liver, lungs and peritoneum [7]. The common sites of distant metastases vary between different subtypes of cholangiocarcinoma. According to the European Network for the Study of Cholangiocarcinoma Registry, which included histologically confirmed diagnoses of cholangiocarcinoma from 2010 to 2019, 32.9% of intrahepatic-cholangiocarcinoma cases showed distant metastasis to lung, whereas 16.5% of distal cholangiocarcinoma cases did. Distal cholangiocarcinoma preferentially metastasized to the liver or peritoneum [8].
Pulmonary metastases typically present as multiple, round, and variably sized peripheral nodules (indicative of hematogenous spread) and diffuse small nodular thickening of the pulmonary interstitium (indicative of lymphatic spread) [9]. Benign diseases such as actinomycosis, anthracosis and pulmonary cryptococcosis can mimic these radiological characteristics.10,11 We present a case of distal common bile duct (CBD) cancer presented with multiple nodules on chest imaging, which was later diagnosed as pulmonary cryptococcosis related to a COVID-19 infection.
CASE
A 64-year-old male was referred to Samsung Medical Center for further evaluation due to abnormal liver function test results detected during an annual health check-up. His medical history included hypertension, diabetes mellitus, and a history of clonorchiasis 20 years ago. The patient reported consuming three bottles of soju three times per week. Initial laboratory finding indicated an alkaline phosphatase level of 428 U/L, gamma-glutamyl transferase level of 1,199 U/L, total bilirubin level of 0.5 mg/dL, aspartate aminotransferase level of 49 U/L, and alanine aminotransferase level of 36 U/L, consistent with a cholestatic pattern of liver function test elevation. Carbohydrate Antigen 19-9 was 46.60 U/mL. Magnetic resonance cholangiopancreatography was performed for further investigation, which revealed a suspected 3.1 cm sized intraductal growing type distal CBD cancer and proximal bile duct dilatation. No evidence of vascular invasion, vascular anatomy variation, or distant metastasis was observed (Fig. 1). Endoscopic retrograde cholangiography demonstrated abrupt cutting of the distal CBD. Multiple endo-biliary biopsies, brush cytology, and endoscopic retrograde biliary drainage were performed, confirming moderately differentiated adenocarcinoma. Positron emission tomography-computed tomography (CT) revealed a hypermetabolic mass involving the distal CBD, with no evidence of regional lymph node involvement or distant metastasis (Fig. 2). The patient was subsequently scheduled for pylorus-preserving pancreaticoduodenectomy (PPPD).
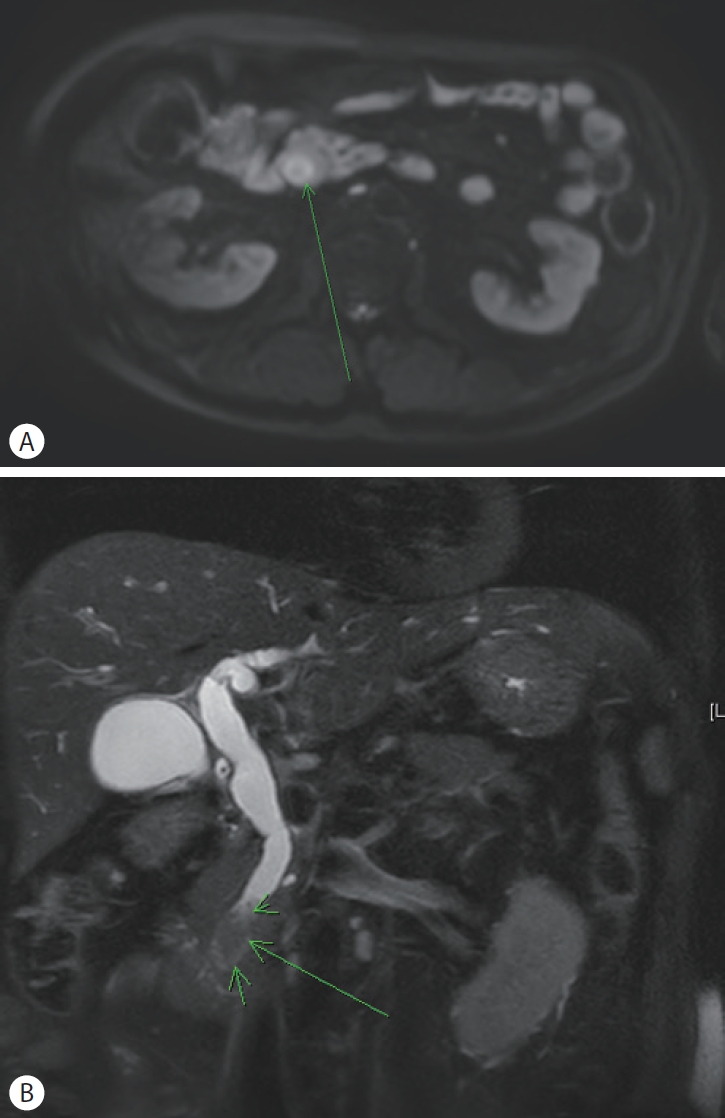
Magnetic resonance cholangiopancreatography. Intraductal growing type distal common bile duct cancer (arrow) with biliary obstruction was found. No evidence of vascular invasion was noted. (A) Axial view synthetic diffusion-weighted imaging. (B) Coronal view T2 weighted image.
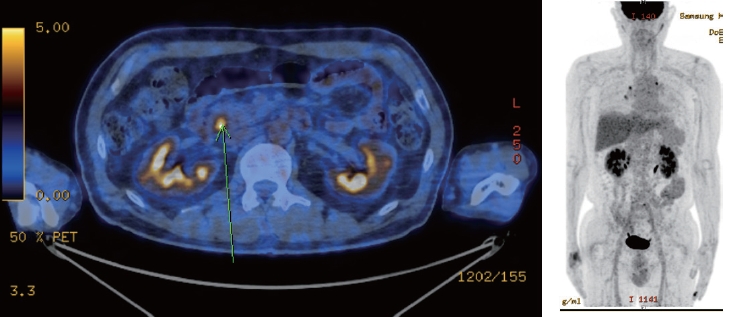
Positron emission tomography-computed tomography. A hypermetabolic mass involving the distal common bile duct (arrow) with no evidence of regional lymph node or distant metastasis was noticed.
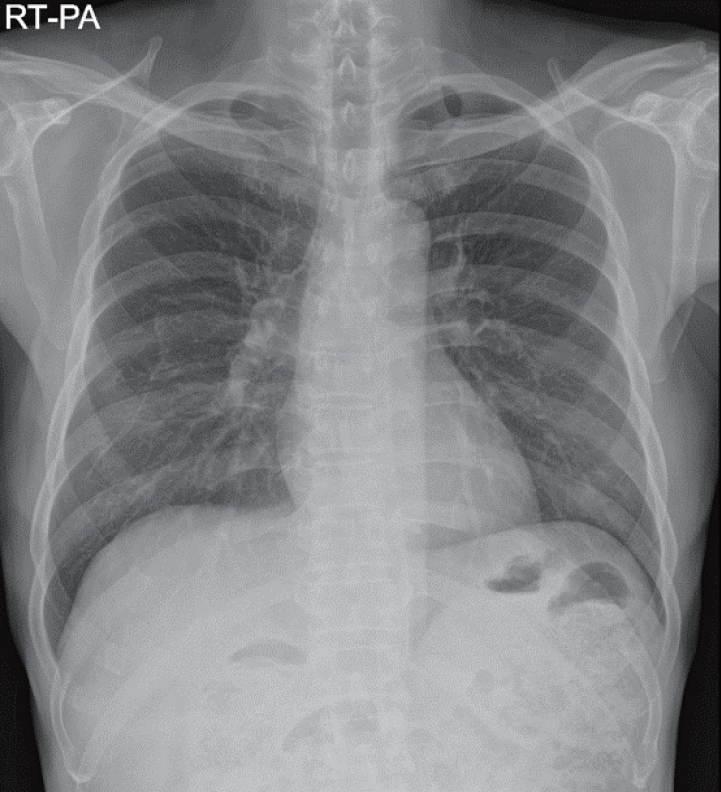
Two months later, a pre-operative check-up chest X-ray revealed multiple nodular lesions in both lungs, suggesting probable metastasis (Fig. 3). A subsequent CT scan revealed multiple solid nodules, with or without a ground-glass halo, in both lungs, which were suggestive of hemorrhagic metastasis (Fig. 4). However, follow-up abdominal CT showed interval decompression of intrahepatic duct dilatation with a plastic biliary stent in place and no change in the lymph nodes at the portocaval space and common hepatic artery.
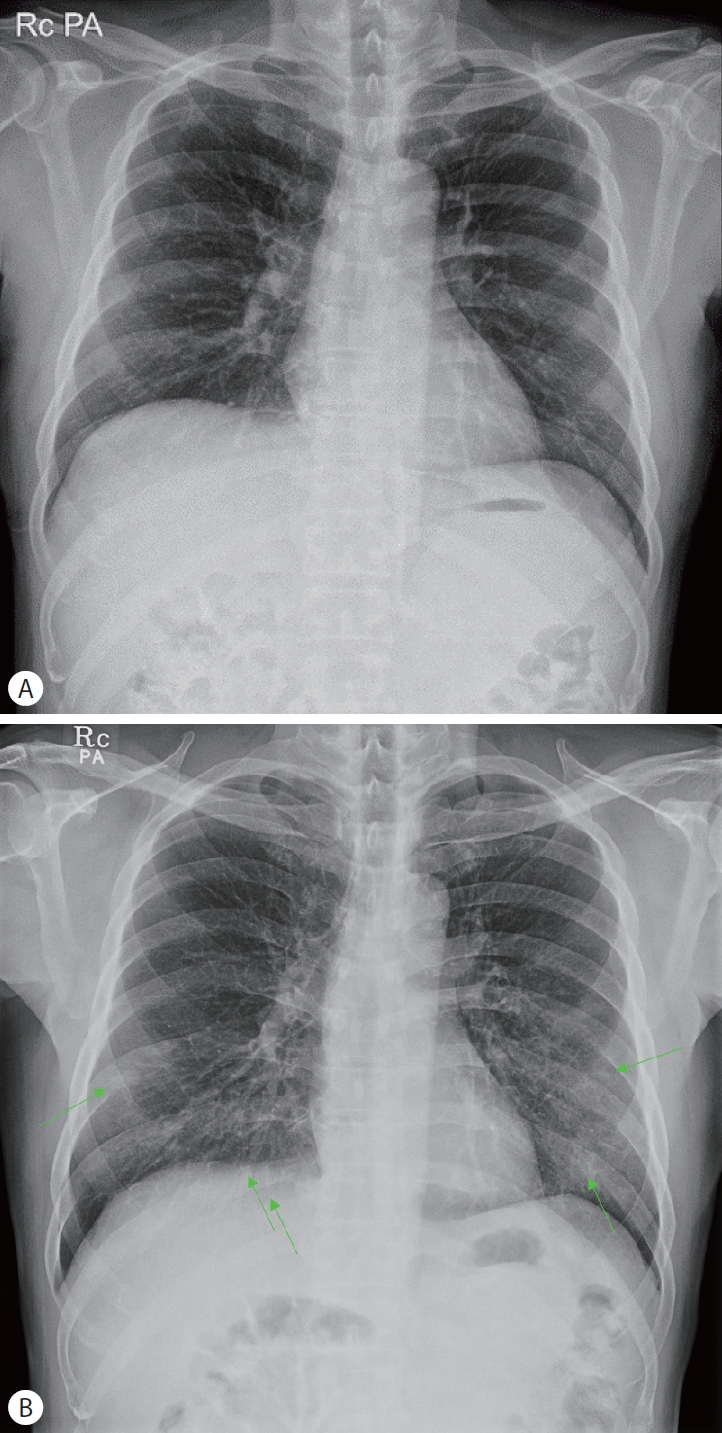
(A) Initial chest radiograph two months prior to operation. There is no significant finding. (B) Pre-operative chest radiograph shows newly detected multiple nodular lesions (arrows) in both lungs.
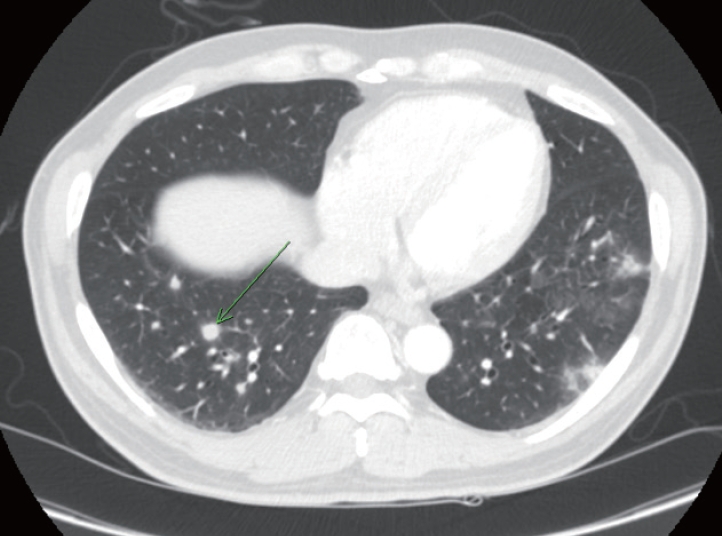
Chest computed tomography. Multiple solid nodules (arrow) with or without ground-glass halo in both lungs were noticed, suggestive of hemorrhagic metastases.
Despite the absence of local progression, the sudden detection of pulmonary metastasis was unusual. Therefore, for pathological verification, a video-assisted thoracoscopic surgical wedge resection of the right lower lobe of the lung was performed. Pathologic examination revealed no evidence of malignancy, instead identifying a non-necrotizing granulomatous lesion. Both Periodic acid-Schiff diastase stain and Grocott or Gomori methenamine silver stain, which detect fungal cell walls, were positive (Fig. 5).
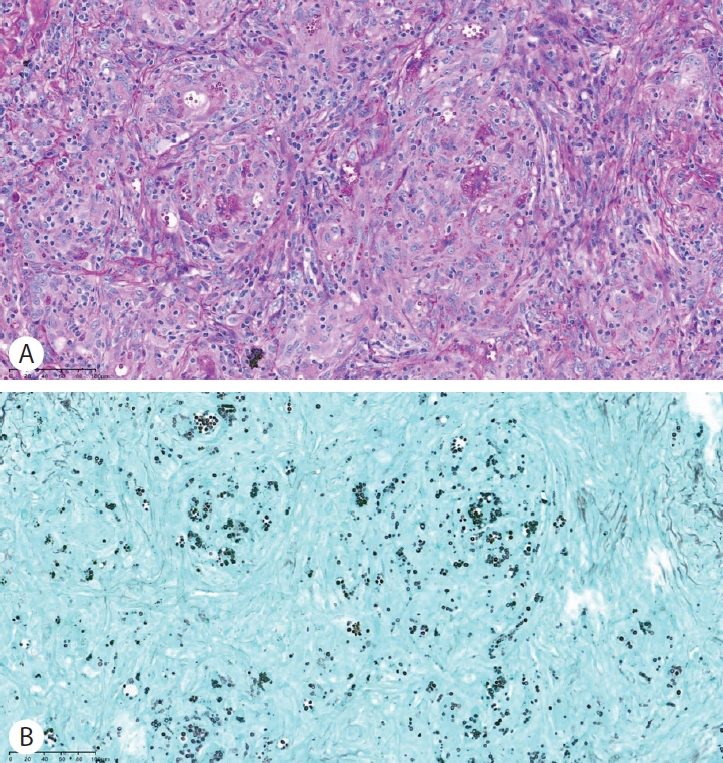
Pathologic findings of lung biopsy. Lung biopsy revealed nonnecrotizing granulomatous lesion with yeast-form organisms consistent with cryptococcal granuloma. (A) Periodic acid-Schiff diastase stain (×100). (B) Grocott’s methenamine silver stain (×100).
Two weeks prior to pre-operation chest X-ray, the patient was diagnosed with COVID-19 pneumonia at a local hospital and was prescribed nirmatrelvir/ritonavir. Based on the patient's history of COVID-19 pneumonia and the pathologic report, cryptococcal antigen blood test was performed, revealing a positive result. The multiple nodules observed on chest imaging were diagnosed as pulmonary cryptococcosis. Consequently, a six-month regimen of fluconazole was initiated, resulting in improvement of lung lesions (Fig. 6).
Chest radiograph after six months of fluconazole shows improvement of multiple pulmonary nodular lesions.
Concurrently, the planned PPPD for distal CBD cancer proceeded as scheduled. Complete resection with grossly and microscopically negative resection margins was performed. Final pathology confirmed distal bile duct cancer of pT1N0M0, stage I and the patient is regularly attending outpatient visits.
DISCUSSION
Cases of pulmonary cryptococcosis are increasingly being identified not only in acquired immune deficiency syndrome patients but also in immunocompetent hosts. The main predisposing factors for cryptococcal infection in immunocompetent hosts include uncontrolled diabetes mellitus, prolonged use of high dose corticosteroids, and use of immunosuppressive drugs, cirrhosis, and malignancy [12]. Recently, there has been an increase in cases of pulmonary cryptococcosis reported after COVID-19 [13,14]. Immune dysregulation caused by the SARS-CoV-2 virus leads to complex alterations in both innate and acquired immunity, increasing the risk of reactivation of latent diseases or the emergence of opportunistic infections, such as fungal infections [14,15].
Primary cancers that frequently spread to the lung include breast cancer, lung cancer, colorectal cancer, uterine leiomyosarcoma, and head/neck squamous cell carcinoma [16]. The presence of multiple pulmonary nodules and cavitation is highly indicative of metastatic disease [11]. Confirming pulmonary metastasis can significantly alter the treatment approach, so it is important to exclude other benign diseases that can mimic metastases.
Pulmonary cryptococcosis presents with various radiological features such as solid nodules, mass with ill-defined or smooth margins, cavitary lesions, pleural effusion, and lymphadenopathy. Specific diagnosis requires histopathological examination. There are several case reports of pulmonary cryptococcosis mimicking pulmonary metastasis in other solid cancers [17,18].
In one of the endemic regions for pulmonary cryptococcosis, India, a similar case was reported where a solitary lung nodule was detected during follow-up after PPPD and adjuvant chemotherapy. Initially suspected to be metastatic, it was ultimately proven to be pulmonary cryptococcosis [19]. This case is the first instance where pulmonary cryptococcosis detected after a recent COVID-19 infection was mistaken for cholangiocarcinoma metastasis.
Despite the presence of multiple nodules observed on chest imaging, there was no evidence of local progression of the distal CBD cancer, which is not typical for its natural course. In addition, one of the predisposing factors for cryptococcal infection, COVID-19 infection, was recent. Video-assisted thoracoscopic surgical biopsy confirmed pulmonary cryptoccosis. This case underscores the importance of thorough evaluation, including detailed history taking, in patients with bile duct cancer in the step of staging.
Notes
Conflict of Interest
The authors have no conflicts to disclose.
