담낭용종에서 악성을 시사하는 예측 인자
Predictive Factors of Malignant Potential in Gallbladder Polyps
Article information
Abstract
초기에 진단된 담낭암은 담낭 용종이나 담낭 결석 같은 다른 양성 질환에 대한 치료 목적으로 담낭절제술을 시행한 이후에 우연히 발견되는 경우가 대부분이다. 의료기술과 향상에 따라 담낭 용종의 발생률이 증가했음에도 불구하고, 담낭 용종에서 악성을 시사하는 인자들에 대한 연구는 부족한 상태이다. 본 연구에서는 437명의 환자 중, 담낭 용종으로 진단된 첫 번째 군의 환자들은 359명이었고, 53명의 담낭선종, 25명의 담낭암으로 진단된 환자들은 두번째 군에 분류하였다. 두번째 군의 환자들이 첫 번째 군의 환자들에 비해서 유의하게 고령(50세 이상), 10 mm 이상의 크기, 담낭벽의 두께 증가를 보였다. 담석 여부는 두 군간에 유의한 차이를 보이지 않았다. 50세 이상, 크기 증가, 담낭벽의 두께 증가 등은 담낭 용종에서 담낭암 또는 전구 병변의 가능성을 시사할 수 있다. 이런 인자들을 가지고 있는 담낭 용종 환자에서 담낭절제술을 고려해야 한다.
Trans Abstract
Background/Aims:
Although the incidence of GB polyps is increasing with improved surveillance, the study of predictive factors of malignant potential has not been sufficient. The aim of this retrospective study is to investigate the predictive factors of malignant potential in GB polyps.
Methods:
Among 3,159 patients with laparoscopic cholecystectomy in Chonbuk National University hospital January 2009 to December 2013, 437 patients confirmed GB polyps pathologically were enrolled. The patients were divided into two groups; one with benign GB polyp and another with GB adenoma and incidental GB cancer.
Results:
Group I with benign GB polyp was seen in 359 patients. On the other hand, 53 patients with GB adenoma and 25 patients with GB cancer in gourp II were identified. The patients in group II had shown a significantly higher incidence of age older than 50 years (53/78, 67.9% vs. 163/359, 45.4%, p=0.001), size larger than 10mm (40/78, 51.3% vs. 37/359, 10.3%, p<0.001), and GB wall thickening (36/78, 46.2% vs. 77/359, 21.5%, p<0.001). The presence of GB stone had not shown significant differences between two groups (26/78, 33.3% vs. 96/359, 26.7%, p=0.378).
Conclusions:
Cholecystectomy should be considered for the patients with GB polyp with these predictive factors.
INTRODUCTION
The prognosis of gallbladder (GB) cancer is very poor because it usually presents at an advanced and incurable stage. 5 year survival rate of progressed GB cancer more than stage III has been estimated below 10%, while 5 year survival rate of stage 0 has been over 80% [1]. Early stage of GB cancer has been usually detected incidentally and the rate of incidental GB cancer after cholecystectomy was reported approximately 0.54-2.1% [2,3].
GB polyp, one of the risk factors of GB cancer, has extremely increasing along with the use of transabdominal ultrasonography. Most of small polyps less than 10mm are benign and remain stable for a long period [4,5]. However, it is difficult to distinguish between GB polyp and early GB cancer. The polypoid lesion larger than 10mm, age older than 50 or combined gallstone have been known predictive factors for malignancy [6]. Current recommendations for managing GB polyps suggest cholecystectomy for the patients presenting symptoms or the patients with risk factors. However, there are lack of large-scale studies on other predictive factors of malignant potential for GB polyp.
The aim of this retrospective study is to investigate the predictive factors of malignant potential of GB polyp compared with GB adenoma and incidental GB cancer.
MATERIALS and METHODS
Among 3,159 patients with laparoscopic cholecystectomy in Chonbuk National University hospital January 2009 to December 2013, 2,665 patients were excluded from the analysis for one of these following reasons: histologically proven acute cholecystitis, chronic cholecystitis or adenomyomatosis without polyp. 33 patients who were diagnosed with other cancer, such as pancreatic cancer, colon cancer, gastric cancer, ampulla of vater cancer, lung cancer, ovarian cancer or breast cancer were excluded. 24 patients already diagnosed with GB cancer before surgery were also excluded. 437 patients with pathologically confirmed GB polyps were enrolled. The patients were divided into two groups: group I - 359 patients with benign GB polyp (76.4%) and group II - 53 patients with GB adenoma (11.3%) and 25 patients with incidental GB cancer (5.3%). The process of the subjects’ selection is shown in a flow diagram (Fig. 1). Group I included the patients with the benign non-neoplastic polyp, such as cholesterol polyp, hyperplastic polyp, or inflammatory polyp.
The demographic and clinical features were collected from the patients’ records retrospectively; age, gender, symptoms such as abdominal pain, dyspepsia, fever, preoperative diagnosis and preoperative procedure such as endoscopic retrograde cholangiopancreatography (ERCP) or percutaneous cholecystostomy (PTC). The patients who had the history of antibiotics treatment for cholecystitis or cholangitis were also checked. Laboratory findings including calcinoembryonic antigen (CEA), carbohydrate antigen 19-9 (CA 19-9), alkaline phosphatase, gamma-glutamyl transferase (GGT), aspartate aminotransferase (AST), alanin aminotransferase (ALT), total and direct bilirubin were performed. Sizes of polyp or tumor were evaluated macroscopically. Radiologic and pathologic finding such as polyp or tumor size, presence of stone, and GB wall thickening were also evaluated. GB wall thickening was identified by imaging studies, such as ultrasonography or computed tomography. Microscopic findings of incidental gallbladder cancer including histological type, differentiation and margin status were evaluated. We used the classification of pathological tumor node metastasis (pTNM) proposed by the American Joint Committee on Cancer (AJCC) for cancer staging.
Statistical calculations were performed with SPSS, version 18.0 for Windows (SPSS Inc., Chicago, IL, USA). The demographic and clinical data of two patient groups were compared using Chi-square test. Laboratory findings were analyzed by student’s t-test. Data are presented as the mean ±SD or percentages. Logistic regression analysis was performed to identify the independent predictive factors for malignant potential. P values less than 0.05 were considered significant.
RESULTS
1. Baseline characteristics
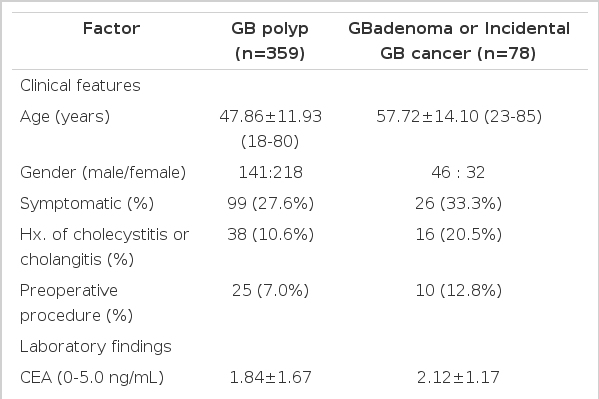
The total number of patients was 437, of whom 37.8 % were male. The median age was 49.6 years (18-85). A total of 359 patients with GB polyp (group I) were identified in our analysis. The mean age at surgery was 47.9 years (range, 18-80), and the female was more common among the group I (female-to-male ratio: 1.54:1) (Table 1). 99 patients had presented symptoms (27.6%), and 38 patients had treated with antibiotics because of cholecystitis or cholangitis (10.6%). Preoperative procedure such as ERCP or PTC was conducted with 25 patients (7.0%). The mean age of the 78 patients with GB adenoma or incidental GB cancer (group II) was 57.7 years (23-85). Male was more common (male-to-female ratio: 1.43:1), and 26 patients had showed symptoms (33.3%). Antibiotics for cholecystitis or cholangitis were prescribed to 16 patients (20.5%), and preoperative procedure was performed in 10 patients (12.8%).
2. Radiologic and pathologic characteristics
Among 359 patients in group I, 332 patients with cholesterol polyp, 25 patients with hyperplastic polyp, and 2 patients with inflammatory polyp were identified. 37 patients had GB polyp larger than 10 mm (10.3%). GB wall thickening and GB stone were observed in 77 and 96 patients (21.5% and 26.7%). 40 out of 78 patients in group II had tumor larger than 10 mm. GB wall thickening and GB stone were observed in 36 and 26 patients (46.2% and 33.3%). 25 patients were diagnosed as an the incidental GB cancer. All tumor histology was identified as adenocarcinoma. According to American Joint Committee on Cancer (AJCC) staging manual, 6th edition, 5 Tis tumors, 6 T1a tumors, 7 T1b tumors, 6 T2 tumors, 1 T3 tumor. Only 1 patient was verified the presence of lymph node involvement. The tumors were well differentiated in 17 patients and moderately differentiated in 8 patients. Cystic duct resection margin was positive in 3 patients.
3. Predictive factors of malignant potential
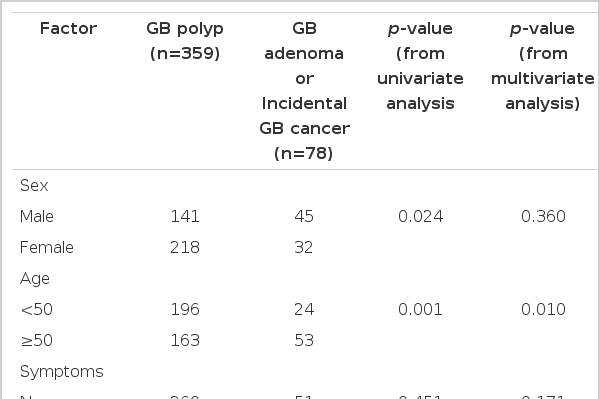
The comparison of clinical characteristics between two groups revealed that the group I had a significantly higher incidence of age older than 50 years (53/78, 67.9% vs. 163/359, 45.4%, p=0.001, odd ratio, 2.22;95%CI, 1.11-4.43) (Table 2). The size larger than 10mm was more frequent in the group II than in the group I (40/78, 51.3% vs. 37/359, 10.3%, p<0.001, odd ratio, 7.09;95%CI, 3.63-13.85). The significant higher incidence of gallbladder wall thickening was found in the group II (36/78, 46.2% vs. 77/359, 21.5%, p<0.001, odd ratio, 2.01;95%CI, 1.03-3.94). Male gender and a history of cholecystitis or cholangitis seemed to increase the risk of GB adenoma or incidental GB cancer, but did not demonstrate any significant differences in the multivariate analysis. The presence of symptoms and preoperative procedure before surgery had shown no significant differences between two groups (p=0.451 and p=0.201). Furthermore, there were no significant differences of the presence of gallstones (26/77, 33.8% vs. 96/359, 26.7%, p=0.378). The laboratory findings were similar in GB polyp, GB adenoma or incidental GB cancer. Tumor markers including CA19-9 or CEA were not helping to diagnosed with incidental GB cancer or GB adenoma (p=0.178 and p=0.705).
DISCUSSION
GB cancer is one of the gastrointestinal or hepatobiliary neoplasms with the worst prognosis. Therefore, it is essential to identify the cancer in early stage. Cholelithiasis is an well-established risk factor for GB cancer, and duration or size of gallstone is associated with increased risk of GB cancer [7-9]. Anomalous junction of pancreaticobiliary duct [10] or porcelain gallbladder [11,12] is additional risk factors for GB cancer. GB polyps are also associated with risk of malignancy.
GB polyps are mostly asymptomatic and symptoms are usually non-specific. Recently, because of wide spread use of transabdominal ultrasonography for health check-up, the incidence of GB polyp is increasing up to 4-5% [13,14]. Most of small GB polyps are benign and remain stable for a long period [9-10]. However, size greater than 10mm of the polyps might be the most important risk factors for GB cancer. In a study of 74 patients with resected gallbladders, cholesterol polyp was found in 44 cases (59%), adenomas in 5 cases (7%), cancers in 6 cases (8%). Almost all (97%) of cholesterol polyps were less than 10mm in diameter. Otherwise 94% of adenoma or carcinomas were greater than 10 mm [15]. Koga et al. [16] reported that 88% of GB cancer patients who underwent cholecystectomy exceeded 10mm in diameter in a retrospective study. Our study have shown similar results that 40 of 78 patients (51.3%) with GB adenoma or incidental GB cancer were greater than 10mm in a diameter while only 37 of 359 patients with GB polyp (10.3%) were over 10 mm (p<0.001).
Cancerous polyps are more frequent in patients older than 50 years of age. Terzi et al. [17] demonstrated that only 27% of patients with benign GB polyp versus 73% of patients with malignant polyp were over 60 years of age. Another study have reported that 26% of the patients with malignant polyp were over 50 years of age, whereas 99% of patient with benign polyp were under 50 years old [18]. Our study also demonstrates the similar (163/359, 45.4% vs. 53/78, 67.9%, p<0.001). Age might be the other crucial consideration for cholecystectomy in GB polyp.
GB cancer may present as focal or diffuse asymmetric wall thickening in 20-30% of cases. In a retrospective study of 78 patients with GB wall thickening demonstrating strong enhancement with irregular contour wall thickening on the computed tomography indicate a possibility of malignancy [19]. We analyzed data about GB wall thickening from pathological and radiological findings and it has significant correlation with malignant potential (77/359, 12.3% vs. 36/78, 46.2%, p<0.001). 75% of patients with GB cancer have been noted to have had gallstones [7-9]. However, there is no significant relation between gallstone and GB cancer in our analysis. GB cancers in our data were detected incidentally and all of them were in early stage. Duration of gallstones might be important for development of GB cancer. A retrospective study of 2,583 patients with gallstone in Minnesota, 5 patients were developed GB cancer after a median follow-up of 13.3 years [20].
In a review of the literature, all patients with gallbladder polyps who are symptomatic, have lesions greater than 10 mm in diameter or have complicating factor such as age over 50 years or concurrent gallstones should undergo surgery [6]. Furthermore, history of inflammation of GB, GB wall thickening could be considered as additional predictive factors for malignancy.
Limitations of this study include the reliance on data obtained from the patients who got surgery. First, patients with GB polyp who were not underwent cholecystectomy, were not included, Second, patients diagnosed with other findings including GB stone or cholecystitis before surgery were included.
In conclusion, although the incidence of GB cancer is relatively low, and most GB polyps have benign natural course, some of GB polyps have its definitely malignant possibility. In this study, male gender, old age (≥50 years), larger size (≥10 mm) and GB wall thickening indicates the possibility of malignant or premalignant lesion in GB polyps. With regular follow up and surveillance, a cholecystectomy should be considered for the patients with these predictive factors of malignant potential in GB polyps.
Notes
Conflict of Interest
The author has no conflicts to disclose.