성인에서 횡격막 탈장에 동반하여 발생한 급성 췌장염의 증례
Acute Pancreatitis Associated with Diaphragmatic Hernia in an Adult
Article information
Abstract
현재까지 보고된 문헌에 따르면 횡격막 탈장에 동반되어 발생한 급성 췌장염의 사례는 드문 것으로 알려져 있다. 횡격막 탈장 시 급성 췌장염이 발생하는 기전은 췌장 자체의 탈장, 탈장으로 인해 췌장의 견인이나 위의 급격한 팽창으로 인해 발생하는 췌장의 허혈로 설명된다.
이 증례는 명치 통증과 호흡곤란을 주소로 내원한 78세 남자 환자에서 영상의학적 검사 및 혈액학적 검사 등을 통하여 췌장의 탈장 없이, 횡격막 탈장에 동반되어 발생한 급성 췌장염을 확인한 증례이다. 환자는 고령임을 감안하여 수술적 치료 없이 보존적 치료만을 시행하였고, 보존적 치료만으로 상태가 호전이 되었으며 34개월 후에도 증상의 재발이 없음을 확인하였다.
현재까지 횡격막 탈장에 의해서 발생한 급성 췌장염에서 정립된 표준 치료는 없으나, 증례를 살펴보면 대부분 위식도 열공 탈장의 수술적 교정을 시행한 후 췌장염이 호전되었고, 수술의 고위험군 환자의 경우 보존적 치료만으로 성공적으로 치료된 경우가 소수 보고되었다.
이 증례를 통하여 저자는 위식도 열공 탈장이 있는 환자에서 급성 췌장염을 유발할 만한 일반적인 원인이 없음에도 불구하고 급성 췌장염이 발생한 경우 횡격막 탈장에 동반한 췌장염의 가능성을 고려해야 함을 설명하고자 하였다.
Trans Abstract
Acute pancreatitis with diaphragmatic hernia is rare, and furthermore, very few were reported in the case without incarceration. The suggested mechanism of acute pancreatitis with diaphragmatic hernia is that herniation of pancreas itself. The other possible mechanism is pancreatic ischemia due to traction after aggravation of hernia or acute distention of stomach. We report a case of acute pancreatitis due to diaphragmatic hernia with no evidence of herniation of pancreas. A 78-year-old male was administered for epigastric pain and dyspnea. The radiologic and laboratory result demonstrated an acute pancreatitis with diaphragmatic hernia without any evidence of herniation of pancreas. The patient was managed conservatively to reduce the hernia and to treat pancreatitis.
INTRODUCTION
Diaphragmatic hernias may occur through the esophageal orifice or other congenital openings. The herniated contents of migration may contain the stomach with various other abdominal organs such as colon, omentum, small intestine, or spleen. Recently, a few literatures reported the association between diaphragmatic hernia and acute pancreatitis [1-4]. Furthermore, few [1] were reported in the case of pancreatitis due to hernia without evidence of incarceration. In this article, we present a case of acute pancreatitis due to diaphragmatic hernia with no evidence of herniation of pancreas.
CASE
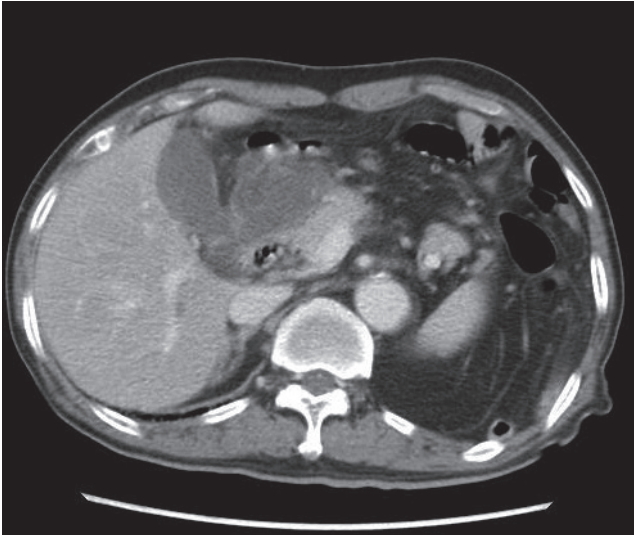
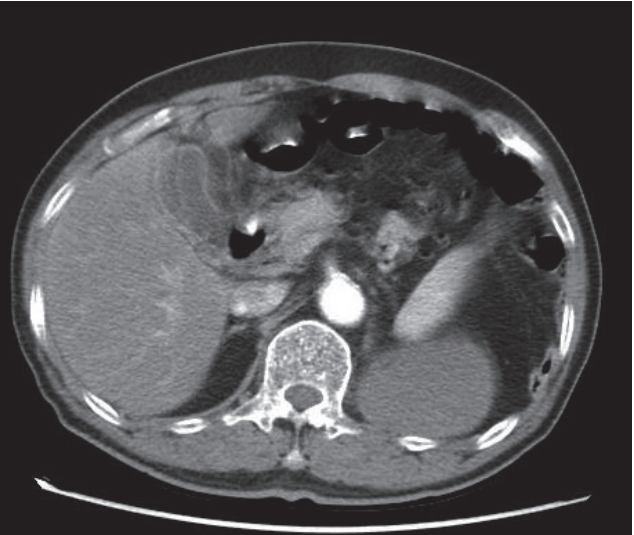
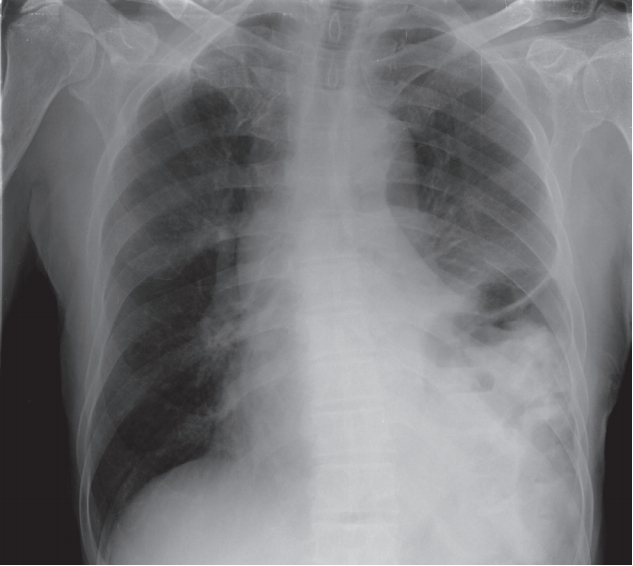
A 78-year-old man presented with one-day history of severe epigastric pain and dyspnea. There was no relevant history of medicine, alcohol or trauma. Scores of years ago, the patient had a history of diaphragmatic hernia at routine check up in primary clinic, but he remained asymptomatic. Abdominal ultrasound 3 months prior in the primary clinic revealed no evidence of cholelithiasis. On physical examination, he had epigastric tenderness and bowel sounds in the left side of the chest. Chest X-ray revealed a large, dome-shaped loops of bowel with air-fluid level in the left hemithorax suggesting left diaphragmatic hernia (Fig. 1). Chest computed tomography (CT) showed extensive left diaphragmatic hernia, resulting in nearly complete collapse or consolidation in the left lung and mediastinal shifting to the right side (Fig. 2). Initial abdomen CT revealed mild pancreatitis which showed suspicious focal pancreatic parenchymal swelling at the pancreatic head area, but no remarkable pancreatic duct dilatation or pancreatic necrosis (Fig. 3). Abdomen CT showed no remarkable common bile duct stone. Serology test at time of initial admission revealed elevated serum amylase of 1,696 U/L (normal 45-108 U/L) and lipase of 2,425.4 U/L (normal 13-60 U/L). A complete blood cell count demonstrated a white blood cell count of 20,250/mm3 (normal 4,000-10,000/mm3), hemoglobin of 19.3 g/dL (normal 13-18 g/dL), and platelet count of 297,000/mm3 (normal 150,000-450,000/mm3). C-reactive protein was 0.71 mg/dL (normal 0-0.3 mg/dL). Blood glucose level was 230 mg/dL (normal 70-110 mg/dL). Other laboratory test workup showed that aspartate aminotransferase 45 IU/L (normal 5-38 IU/L), alanine aminotransferase 126 IU/L (normal 4-43 IU/L), alkaline phosphatase 313 IU/L (normal 102-333 IU/L), gamma glutamyl transpeptidase 290 U/L (normal 11-75 U/L), total bilirubin 2.70 mg/dL (normal 0.2-1.2 mg/dL) and triglyceride 63 mg/dL (normal 30-150 mg/dL). Immunologic data including serum immunoglobulin G, A, M, E levels were normal, and antinuclear antibody levels were negative, and anti-neutrophil cytoplasmic antibody, anti-mitochondria antibody, antismooth muscle antibody levels were negative. Serum IgG4 was not elevated at 0.27 g/L (normal 0.06-1.21 g/L) with total IgG 959 mg/dL (normal 700-1,600 mg/dL). Viral marker revealed negative HBs Hepatitis B surface antigen (HBsAg) positive Hepatitis B surface antigen (HBsAg) Hepatitis B surface antibody (HBsAb) and negative Hepatitis C antibody (HCV Ab) Ab. Arterial blood gas analysis showed bicarbonate retention up to 68.3 mmHg and the patient showed decreased mentality and he was initiated invasive ventilation in intensive care unit. The patient was treated with nasogastric tube drainage with intravenous fluid and empirical antibiotics, and the status of general condition was gradually recovered. On 3rd hospital day, follow-up chest posteroanterior view demonstrated that interval regression of left lung collapse and the volume of hernia was reduced (Fig. 4), and successful extubation was performed. On 10th hospital day, physical examination revealed no signs of any peritoneal irritation and abdominal pain, then a liquid or soft diet was started. The follow-up serology test demonstrated near normal level of serum amylase 119 U/L, and lipase 106 U/L. On 25th hospital day, follow-up chest xray showed interval re-expansion of left lung (Fig. 5), and abdomen CT demonstrated the sequela of acute pancreatitis, such as peripancreatic pseudocyst with the size 12 cm (Fig. 6). We recommended that the repair of the diaphragmatic hernia would be required. However, the patient refused to undergo surgery. The patient was discharged with no symptoms and a plan to follow-up for pancreatitis with diaphragmatic hernia. Thirty four months later, the patient remained asymptomatic and follow up CT was not performed because of patient’s refusal.

Chest X-ray showed a large, dome-shaped bowel gases in the left thorax indicating a left diaphragmatic hernia.
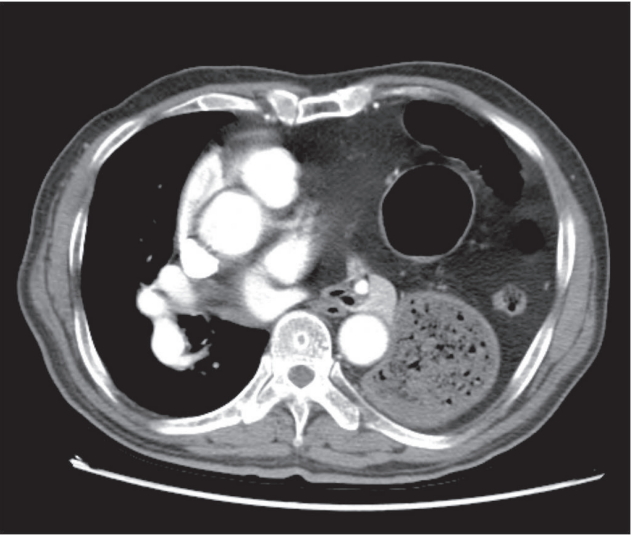
A chest computed tomography demonstrated left diaphragmatic hernia with content of stomach and small bowel with mediastinal shifting to the right side.
Abdomen computed tomography revealed focal pancreatic parenchymal swelling at the pancreatic head area suspicious of acute pancreatitis.

Follow-up chest X-ray on 3rd hospital day demonstrated that interval regression of left lung collapse and the volume of hernia in the left thorax was reduced.
Follow-up chest X-ray showed an increase of the volume of left lung and a decrease of bowel gases in the left thorax.
DISCUSSION
Acute pancreatitis associated with diaphragmatic hernia is an extremely rare condition in literature. The suggested mechanism is that herniation of pancreas itself may produce the traumas in vascular segmental branches or biliopancreatic conducts as well as sign of obstruction of the pancreatic duct [2,3]. The acute pancreatitis due to herniation could result in strangulation or incarceration of gland with or without pancreatic volvulus [2-4]. Another possibility is pancreatic ischemia due to traction after aggravation of hernia or acute distension of the stomach [1] which might be the cause of our case. The fact that the pancreas itself was not evident among the hernia content, and the main lesion of pancreatitis is the head of pancreas which is far from the site of herniation, may support the favor of the latter opinion that the cause of pancreatitis is pancreatic ischemia due to traction. The weak point of our case is that we couldn’t perform the magnetic resonance cholangiopancreatography or endoscopic ultrasonography because of poor patient’s condition. However, abdomen ultrasonography prior to admission revealed no evidence of gallstone, and medical treatment with expansion of lung alone had improved the pancreatitis. Accordingly, the cause of pancreatitis might be related with hernia itself. Although, fortunately, the conservative approach to reduce the hernia and to treat pancreatitis has an effect in our case, we believe that a fundamental therapeutic approach is repair of diaphragmatic hernia especially in case of acute pancreatitis associated with diaphragmatic hernia.
Given the limited number of cases reported so far [1-9], the most appropriate treatment of acute pancreatitis secondary to pancreatic herniation has not yet been established. Historically, patients were immediately treated with hiatal hernia repair [2]. Whereas, some recent reports [3,6,8] indicate that patients who have failed surgery due to high surgical risk or patient rejection have been successfully treated with supportive care (e.g., intravenous fluid supplementation, analgesia, early enteral feeding). However, in severe cases related to incarceration, perforation, or unresponsiveness to medical therapy, surgical management should be performed. Although they did not find pancreatitis cases which are similar to ours, Kohn et al. [9] reported in their literature that all symptomatic paraesophageal hernia should be repaired, particularly those with acute obstructive symptoms or those that have undergone volvulus.
The table 1 shows other cases of acute pancreatitis with diaphragmatic hernia and their treatment and prognosis. The recurrence rate of symptomatic paraesophageal hernia without surgical treatment is low, so the role of elective surgical reduction is uncertain. In addition, most affected patients are older and have significant comorbidities, making them poor operative candidates. Therefore, the decisions about surgical treatment should be made to individual patients. Elective repair may be considered in younger patients with low perioperative risk to prevent future complications.
When we encounter the patients with a history of hiatal hernia, diagnosed as pancreatitis without the evidence of the common causes of pancreatitis such as alcohol, stone, trauma, immunologic reaction, the diaphragmatic hernia should be considered for the underlying case of unknown pancreatitis. In addition, without evidence of herniation of pancreas, acute pancreatitis due to diaphragmatic hernia could occur.
Notes
Conflict of Interest
The authors have no conflicts to disclose.