수술 후 확인된 담낭 육종양암종
Gallbladder Sarcomatoid Carcinoma Diagnosed after Surgery
Article information
Abstract
육종양암종은 담낭에서 드물게 발생하는 암으로 육종과 암종의 성격을 동시에 지니기 때문에 공격적이고 빠른 진행을 보이며 수술적 치료 이외에 정립된 보조 요법이 없어 예후가 불량하다고 알려져 있다. 본 저자들은 82세 남자 환자가 옆구리 통증을 주소로 복부 전산화단층촬영을 시행 후 확인된 담낭암에 대한 감별 진단을 시행하였고 다양한 영상학적 검사를 시행하였으나 그 성격을 예측할 수 없었다. 수술 후 병리조직검사 중 면역 화학 염색을 시행한 결과 시토케라틴과 비멘틴에 양성을 보이는 담낭육종양암종의 증례를 경험하였기에 보고한다. 환자는 정립된 항암 보조 요법이 없는바 재발 가능성을 줄이기 위한 방사선 치료를 계획하고 있다.
Trans Abstract
Sarcomatoid carcinoma is rarely diagnosed as gallbladder cancer. Its aggressive nature, due to the characteristics of both sarcoma and carcinoma, results in a poor prognosis. We report a case of gallbladder sarcomatoid carcinoma in an 82-year-old male who was referred to our hospital for evaluation of gallbladder cancer observed on abdominopelvic computed tomography. The characteristics of the cancer were not confirmed after several imaging modalities. The surgically resected tumor was positive for both cytokeratin and vimentin as revealed via immunohistochemical staining, and a sarcomatoid carcinoma was finally diagnosed. The role of chemotherapy has not yet been identified. Therefore, radiation therapy is planned to reduce the risk of recurrence.
INTRODUCTION
Primary gallbladder cancer accounts for 0.6% of all cancers reported worldwide [1]. In Korea, gallbladder and other biliary tract carcinomas are reported in 2.9% of all cancers, with a crude incidence of 14.4 out of 100,000 people, and it is the fifth most common cancer of the gastrointestinal tract [2]. The most common histological type of gallbladder neoplasm is adenocarcinoma, which accounts for 98% of all cases [3]. Gallbladder sarcomatoid carcinoma is rare with an incidence rate of less than 1% [4]. Sarcomatoid carcinoma is a mixture of sarcomatous component with an epithelial portion originating from the carcinomatous component. Sometimes, a sarcomatoid carcinoma is composed of only a heterologous sarcomatous component [4]. It aggressively spreads from the primary site to the metastatic sites and can occur throughout the body, with the most common site being the lungs [5]. Radical or palliative surgery is the standard treatment. However, its prognosis is poor due to recurrence [6]. Even adjuvant chemotherapy has an uncertain efficacy [7]. We present a case of gallbladder cancer that was diagnosed as sarcomatoid carcinoma based on pathological findings after surgery.
CASE
An 82-year-old man visited a local hospital for evaluation of right flank pain. Abdominopelvic computed tomography was performed to evaluate symptoms. Gallbladder perforation due to gallbladder cancer has also been suggested. Prostate enlargement also suggested the aggravation of benign prostate hyperplasia (BPH) or prostate cancer (Fig. 1).
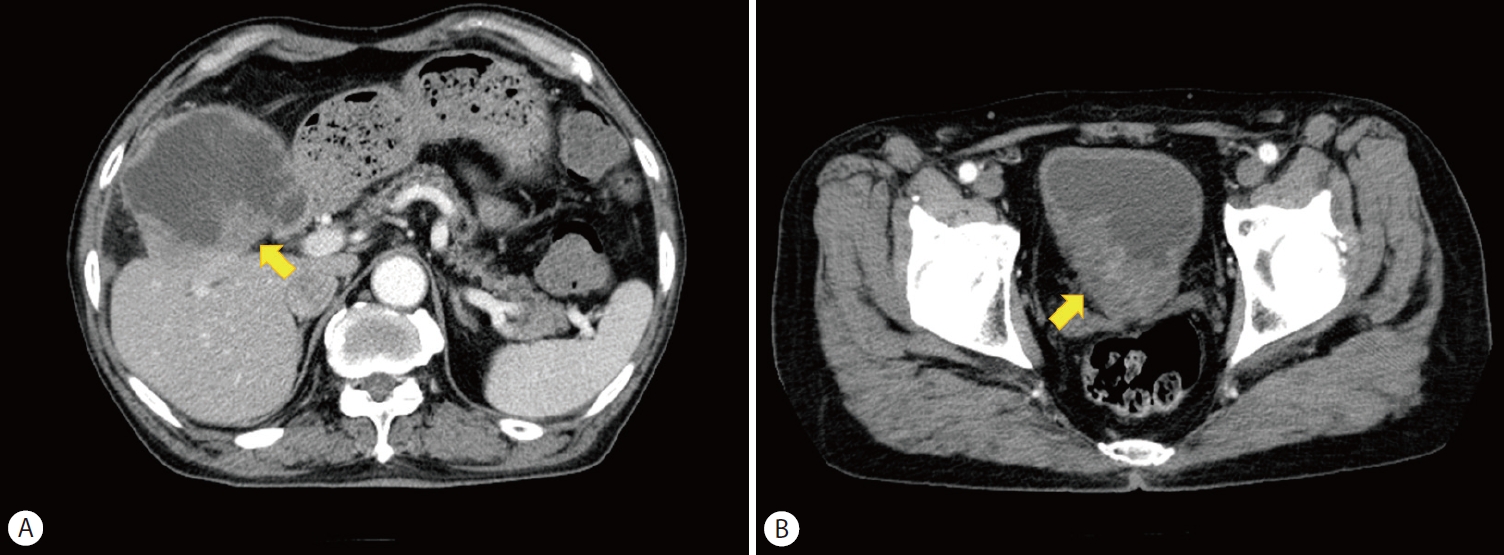
Abdominopelvic computed tomography. (A) Diffuse-enhancing irregular wall thickening of the gallbladder was observed with distension, direct invasion to the liver, and sealed-off perforation of the gallbladder cancer. (B) Enlarged prostate gland with heterogeneously enhancing mass in the right lobe was observed.
The patient was referred to Soonchunhyang University Hospital for further evaluation and management of the gallbladder cancer. The patient’s relevant medical history included chronic hepatitis B, BPH, esophageal papilloma, and recurrent liver abscess. Surgical history included transurethral resection of the prostate for BPH in 2003 and endoscopic mucosal resection of the esophagus for papilloma in 2009. His social history was unremarkable.
Systemic examination revealed nonspecific findings. The pain in the right flank subsided. On physical examination, the patient’s vital signs were stable. Complete blood count examination revealed mild anemia, with a hemoglobin count of 11.3 gm/dL. On chemical analysis, amylase and lipase levels were elevated to 131 and 66 U/L, respectively. Erythrocyte sedimentation rate and C-reactive protein levels were elevated at 120 mm/h and 2.11 mg/L, respectively. Tumor markers revealed elevated carcinoembryonic antigen at 9.7 ng/mL. Viral markers were hepatitis B surface antigen positive and anti-hepatitis B-negative. Chest radiography revealed nonspecific findings, whereas a simple abdominal radiograph revealed mild paralytic ileus.
Positron emission and computed tomographies were performed to evaluate the metastatic lesions for a staging workup (Fig. 2). No metastatic lesions were observed. Fluorodeoxyglucose uptake by the prostate cannot be used to rule out prostate cancer. Contrastenhanced endoscopic ultrasonography was performed to identify the characteristics of the gallbladder mass (Fig. 3). Unlike the usual gallbladder cancers, such as adenocarcinoma, no enhancement was observed in any phase, which suggests a rare histologic characteristic of the mass of the gallbladder. Biliary and pancreatic dynamic magnetic resonance imaging was performed to evaluate the direct invasion of the mass into nearby organs and lymph node metastasis. Previous imaging studies have confirmed this result. A few enlarged lymph nodes were also observed suggesting lymph node metastasis (Fig. 4).
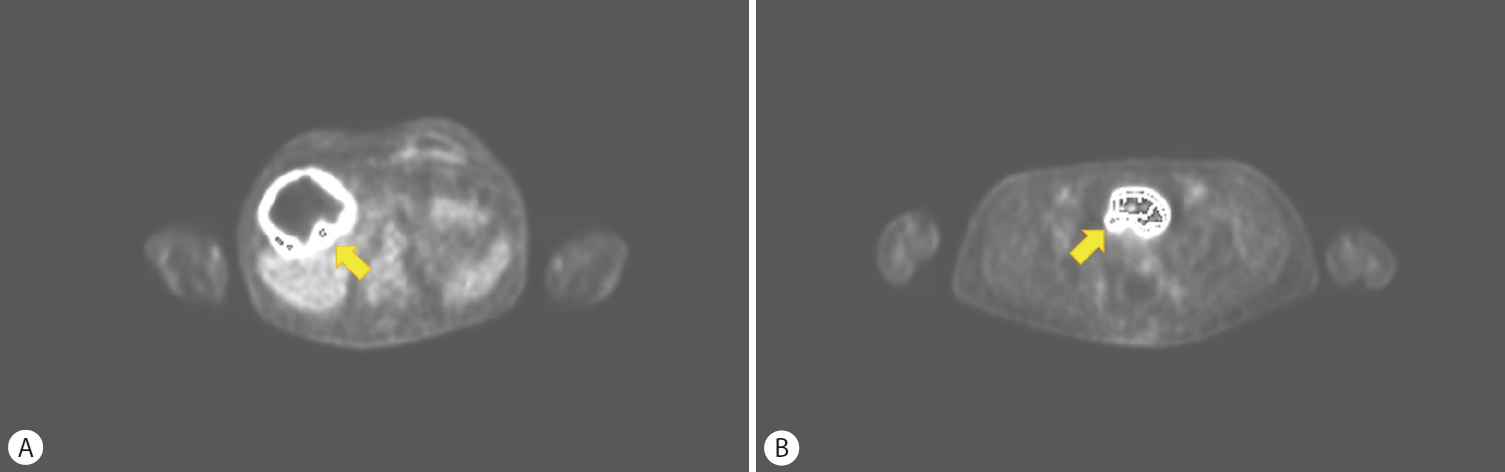
Positron emission tomography computed tomography. (A) Fluorodeoxyglucose (FDG) uptakes on the gallbladder mass. (B) FDG uptakes on the prostate gland.

Contrast-enhanced endoscopic ultrasonography (EUS). (A) Initial EUS: Irregular wall thickening of the gallbladder was observed with mass inside, destroyed borderline of the wall of the gallbladder and liver. Gallbladder stone and sludge were also noted. (B) Arterial phase of EUS: No enhancement was observed 35 seconds after SonoVue contrast injection. (C) Portal phase of EUS: No enhancement was observed 62 seconds after SonoVue contrast injection.
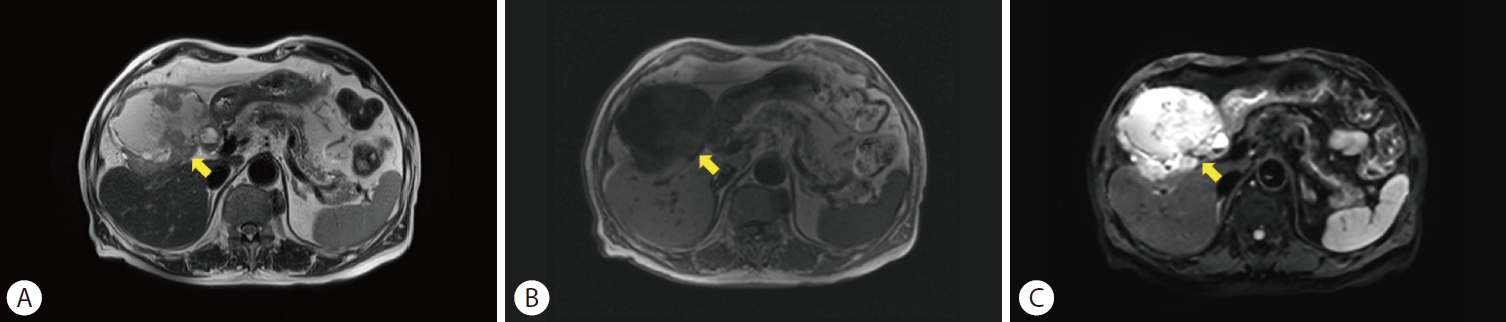
Biliary and pancreas dynamic magnetic resonance imaging (MRI). Diffuse-enhancing irregular wall thickening of the gallbladder was observed with direct invasion to the liver and sealed-off perforation of the gallbladder. (A) Axial T2-weighted MR image showed irregular gallbladder wall thickening and polypoid gallbladder mass, which were mildly hyperintense relative to the liver parenchyma. (B) Axial T1-weighted image showed the mass isointense to the liver parenchyma. (C) Diffusion-weighted image showed high signal intensity of the wall thickening from restricted diffusion.
The final diagnosis after imaging studies was gallbladder cancer with lymph node metastasis. However, the characteristics of the mass were not identified. A combined general surgery and urology operation was planned on hospital admission day 14. Radical cholecystectomy, gallbladder bed resection, radical lymph node dissection, bile duct resection, and Roux-en-Y hepaticojejunostomy were planned along with a prostate biopsy.
The gallbladder specimen consisted of the entire gallbladder and part of the liver. The serosal surface was covered with a brownish exudate. The gallbladder wall thickened and measured 0.3 cm. The lumen contained calculi. The mucosa was not bile stained or ulcerated. Gallbladder cancer had directly infiltrated the liver, based on gross and microscopic findings (Fig. 5). The characteristics of both adenocarcinoma and sarcoma were observed through usual and special staining of cytokeratin. Sarcomatoid carcinoma-specific staining for vimentin was positive. All the dissected lymph nodes showed reactive hyperplasia. The final diagnosis was a biopsy-proven sarcomatoid carcinoma without lymph node metastasis. A prostate biopsy suggested BPH.

Gross specimen and pathologic findings. (A) Gross specimen after radical cholecystectomy; green ink was used for the gallbladder (GB), and black ink was used for the liver. Irregular excavated lesion was observed with thickening and directly extending to the liver. (B) Deeply infiltrating tumor directly invading the liver was observed through microscopy (hematoxylin and eosin stain, ×12.5). (C) Gland forming adenocarcinoma and atypical spindle cells on the sarcomatous area were observed through microscopy (hematoxylin and eosin stain, ×40). (D) Malignant glandular epithelium and spindle were positive for cytokeratin (cytokeratin, ×100). (E) Sarcomatous spindle cells were positive for vimentin (vimentin, ×100).
Adjuvant radiation therapy is planned to lower the chance of local recurrence as adjuvant chemotherapy does not have evidence of efficacy. The patient was followed up in the outpatient department.
DISCUSSION
Early gallbladder cancer rarely presents with symptoms making early diagnosis difficult. It presents the same difficulty as sarcomatoid carcinoma is a rare gallbladder cancer. In addition, sarcomatoid carcinoma has aggressive progression, which requires earlier diagnosis than other gallbladder cancers. However, no other differential diagnostic modalities exists for distinguishing sarcomatoid carcinoma from other gallbladder cancers. Only the special pathological staining technique of cytokeratin and vimentin can distinguish sarcomatoid carcinoma after surgery.
Owing to its rarity, adjuvant and palliative treatments for sarcomatoid carcinoma are not known. Surgical resection is the treatment of choice. However, no evidence-based treatment exists for postoperative recurrence.
To overcome the limitations of diagnosis and treatment, more cases should be collected to study the physiology and pathology of sarcomatoid carcinoma of the gallbladder.
Notes
Conflicts of Interest
The authors have no conflicts to disclose.
