췌장염에 동반된 가성동맥류 파열의 색전술을 이용한 치료
Pseudoaneurysmal Rupture Associated with Pancreatitis Treated with Transarterial Embolization: A Case Series
Article information
Abstract
췌장 가성동맥류는 췌장염이나 췌장 수술과 연관되어 종종 생명을 위협하는 합병증으로 알려져 있다. 췌장 가성동맥류가 파열되면 치명적인 출혈을 유발할 수 있으며 높은 사망률과 관련이 있기 때문에 임상적 의심과 조기 진단이 환자의 임상 경과를 호전되게 할 수 있는 중요한 역할을 한다. 가성동맥류의 치료법 중 하나로 알려진 색전술은 효과적일 수 있으나, 췌장염과 관련된 가성동맥류 파열 환자의 색전술 치료 결과에 대한 국내 연구는 적다. 이에 췌장염으로 인한 가성동맥류 파열을 진단받고 색전술로 성공적으로 치료받은 환자들에 대한 증례를 보고한다.
Trans Abstract
Pancreatic pseudoaneurysm is a potentially life-threatening complication often associated with pancreatitis or pancreatic surgery. As the rupture of pancreatic pseudoaneurysms can lead to catastrophic bleeding and is associated with high mortality rates, clinical suspicion and early diagnosis are essential to improve patient outcomes. In the management of pseudoaneurysms, transarterial embolization (TAE) could be effective; however, there have been limited local studies on the outcomes of TAE for patients with pseudoaneurysm rupture associated with pancreatitis. Here, we describe patients who were diagnosed with pseudoaneruysm rupture associated with pancreatitis and treated with TAE.
INTRODUCTION
Pseudoaneurysm is a complication that could occur in patients suffering from acute or chronic pancreatitis [1,2]. This formation, a result of pseudocyst pressure and enzymatic action, can lead to pseudoaneurysmal bleeding, which is a life-threatening condition with a mortality rate of up to 37% [3]. It has been reported that this type of bleeding occurs in 5-10% of patients who have pseudocysts associated with chronic pancreatitis [2].
The clinical manifestation of pancreatitis-associated pseudoaneurysm could vary, ranging from asymptomatic to periumbilical pain, melena, hematochezia, and hemodynamic instability. Accordingly, it is important to accurately and timely diagnose pseudoaneruysm rupture through imaging studies [4].
As conservative management of active hemorrhage due to pseudoaneurysm is known to be associated with a high mortality rate of up to 52%, interventional treatment, such as transarterial embolization (TAE), is required [2]. Although TAE is currently considered as a primary therapeutic option for patients with pseudoaneurysms associated with pancreatitis [5], there have been limited studies on the etiology of pseudoaneurysm rupture associated with pancreatitis and the outcomes of TAE. Therefore, we aimed to present a case series of patients with pseudoaneruysm rupture associated with pancreatitis, which were ultimately treated with TAE.
CASE
Here, 4 patients were diagnosed with pancreatic pseudoaneurysm and treated with TAE, whose data are summarized in Table 1 and 2.

Baseline characteristics and outcomes of patients diagnosed with pancreatic pseudoaneurysmal rupture treated with trans-arterial embolization
1. Case 1
A 71-year-old male visited our gastroenterology department with a complaint of weight loss (10 kg over a month). He had a history of admission due to acute alcoholic pancreatitis 4 years ago in DMC Bundang Jesaeng General Hospital. He consumed alcohol daily (1 bottle of soju per day) for the past 3 years. The patient was admitted for the evaluation of weight loss. Vital signs were stable (130/80 mmHg, 70 HR/min, 36.5℃), and initial laboratory findings showed anemia (hemoglobin: 12.2 g/dL [13-17 g/dL]), elevated C-reactive protein (12.54 mg/dL [0.00-0.80 mg/dL]), and elevated amylase (61 U/L [28-100 U/L] and elevated amylase (61 U/L [28-100 U/L]) and lipase level (98 U/L [13-60 U/L]). Accordingly, abdomino-pelvic computed tomography (AP-CT) was performed, which showed chronic pancreatitis with an approximately 1.6 cm-sized pseudoaneurysm at the anterior portion of the pancreatic pseudocyst, indicating the possibility of rupture of a branch of the splenic artery (Fig. 1A). Accordingly, we decided to perform TAE as a preventive measure considering the potential risk of additional bleeding that could lead to complications such as rupture. This intervention was successfully performed without any complication (Fig. 2A). The patient was successfully discharged from the hospital with serial follow-up.

Computed tomography images of hemorrhage from pancreatic pseudoaneurysmal rupture (arrow). (A) An 1.6 cm sized pseudoaneurysm at anterior portion of pancreatic pseudocyst, located at the pancreatic body and tail portion, (B) hematoma within the pancreatic head portion, and (C) hematoma in pancreas tail.
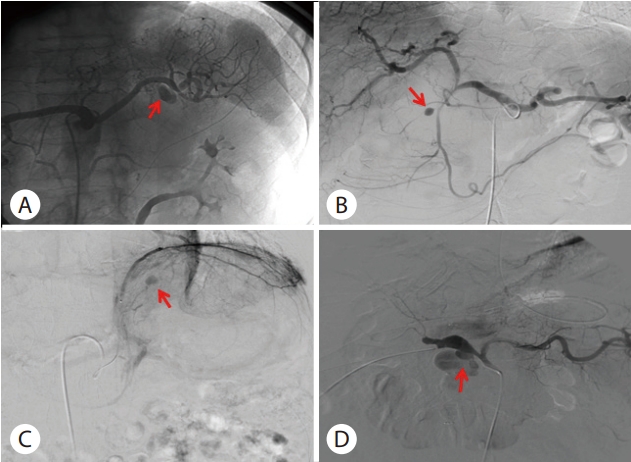
Angiographic images of pseudoaneurysm. (A) An 1.6 cm sized pseudoaneurysm at one branch of splenic artery (arrow) (Case 1). (B) An 1 cm sized pseudoaneurysm from duodenal branch of gastroduodenal artery (arrow) (Case 2). (C) An 1.3 cm sized pseudoaneurysm in branch of left subphrenic artery (arrow) and splenic artery (Case 3). (D) A 4.2 cm sized large pseudoaneurysmal change of common hepatic artery (arrow) with active extravasation of contrast media (Case 4).
2. Case 2
A 35-year-old male was admitted to our hospital due to worsening abdominal pain following a traffic accident 3 days ago. The patient had a history of several admissions to our hospital for acute alcoholic pancreatitis. Before his admission to the hospital, he was previously diagnosed with chronic pancreatitis, which was identified by pancreatic parenchymal atrophy combined with pancreatic duct dilatation on the past CT scan. Four days prior to the hospital visit, the patient was in a car accident where he was struck in the epigastric area by the steering wheel, which caused and exacerbated his recurrent abdominal pain. Upon admission to the emergency department, laboratory findings showed elevated value of amylase (895 U/L [28-100 U/L]) and lipase (1,353 U/L [13-60 U/L]). To evaluate the cause of abdominal pain, AP-CT was performed, and it revealed pancreatic head swelling and peripancreatic fluid collection, consistent with acute necrotizing pancreatitis. However, arterial phased CT showed extravasation of contrast media within newly occurred hematoma around the pancreatic head portion (Fig. 1B). For the evaluation and management of the active bleeding, transarterial angiography was performed, which revealed a 1 cm-sized pseudoaneurysm in one of the duodenal branches of the gastroduodenal artery, likely related to the recent trauma. Therefore, immediate embolization using microcoils was performed on the main gastroduodenal artery along with the pseudoaneurysm site (Fig. 2B). After following supportive management, his abdominal pain improved, and the patient was successfully discharged from the hospital without any complications.
3. Case 3
A 59-year-old male with a history of chronic alcoholism and multiple episodes of alcoholic acute pancreatitis presented to the emergency department with acute onset epigastric pain. He was diagnosed with recurrent necrotizing pancreatitis based on AP-CT and laboratory findings (amylase: 101 IU/L, lipase: 170 IU/L) and admitted to the gastroenterology department for further management. On the seventh day of hospitalization, a sudden decrease in blood pressure and hemoglobin levels occurred with a clinical suspicion of internal bleeding. AP-CT was performed again, revealing hemorrhage of the pancreatic cyst (Fig. 1C). Following consultation with the radiology department, angiography was performed, which identified two pseudoaneurysms in the branches of the left subphrenic artery and splenic artery (Fig. 2C). Embolization was successfully performed immediately to manage the pseudoaneurysms to prevent further hemorrhage. On the eighth day after embolization, the patient eighth discharged from the hospital, exhibiting an improvement in general health and stable hemoglobin levels.
4. Case 4
A 70-year-old male patient with a past medical history of hypertension presented to the outpatient urology department complaining of left flank pain, and AP-CT was performed, which showed a prominent ampulla of Vater (AoV) (Fig. 3A) with diffuse intrahepatic duct dilatation (Fig. 3B), raising suspicion for possible AoV cancer. Endoscopic retrograde cholangiopancreatography (ERCP) was performed, and after endoscopic sphincterotomy, a villous lesion was identified at the distal common bile duct (Fig. 3C), which was confirmed as an adenocarcinoma on histologic examination. Accordingly, the patient underwent pylorus-preserving pancreaticoduodenectomy (PPPD) for the management of the cancer (Fig. 3D). However, on the twelfth day post-surgery, he began to complain of sudden abdominal distension and abdominal pain, and he started to develop a fever of 38℃. To identify the cause of the fever and abdominal discomfort, AP-CT was performed, and the patient was diagnosed with acute pancreatitis. A decision was made to maintain fasting and conservative therapy while closely monitoring his condition. However, on the fifteenth post-operative day, he suddenly had massive melena with a significant decrease in hemoglobin levels from 10.1 g/dL to 6.9 g/dL. To evaluate and manage the active bleeding, emergent angiography was performed, which showed a 4.2 cm-sized large pseudoaneurysm in the common hepatic artery, followed by therapeutic embolization (Fig. 2D). Although technical success of embolization was achieved, his systemic condition worsened on the following day, resulting in multiple organ failure, and he ultimately expired after 25 hours after the embolization.

Images of case 4 patient. (A) Computed tography shows prominent ampulla of Vater (AoV) and (B) diffuse intrahepatic dilation and common bile duct dilatation. (C) Endoscopic image of AoV mass af ter endoscopic sphincteromy, which was revealed as an adenocarcinoma in histology. (D) Gross specimen after pyloruspreserving pancreaticoduodenectomy.
DISCUSSION
Pancreatic pseudoaneurysm is a potentially life-threatening complication often associated with pancreatitis or pancreatic surgery. As the rupture of pancreatic pseudoaneurysms can lead to catastrophic bleeding and is associated with high mortality rates, clinical suspicion and early diagnosis are essential to improve patient outcomes [3].
Pseudoaneurysms are associated with pancreatitis in approximately 10% of patients and occur due to enzymatic insult to peripancreatic arteries or erosion of a pseudocyst into adjacent visceral arteries [1]. When an inflamed pancreas leaks pancreatic enzymes, it can cause the enzymatic autodigestion of vascular walls, leading to diffuse bleeding, extensive necrosis, or pseudoaneurysm formation. Additionally, a visceral artery can become embedded within the wall of a pseudocyst, transforming it into a pseudoaneurysm [2].
The splenic artery is the most commonly affected artery (60-65%) due to its contiguity with the pancreas, followed by the gastroduodenal (20-25%), pancreaticoduodenal (10-15%), hepatic (5-10%), and left gastric (2-5%) arteries [6]. In our case series, 2 of 4 patients (50%) had pseudoaneurysms affecting the splenic artery, consistent with previous findings, whereas the other 2 patients had pseudoaneurysms affecting the gastroduodenal artery or hepatic artery. Further research is needed considering that the prognosis can vary depending on the location of the arteries.
Previous studies have reported the occurrence of pseudoaneurysms arising from pancreatitis. Golzarian et al. [7] evaluated TAE as a therapeutic modality for 9 patients with 13 pseudoaneurysms secondary to pancreatitis, among whom 8 patients had chronic pancreatitis. According to domestic reports, there were 27 cases where a preceding cause could be analyzed; among them, 23 cases involved chronic pancreatitis, and 4 cases involved acute pancreatitis. Of these cases, 19 cases had a discernible cause for pancreatitis, which was chronic alcohol consumption [8]. In our case series, the etiology of 2 patients was related to acute pancreatitis (Case 1 and Case 3). The etiology of 1 patient was related to traumatic damage to the pancreas in the presence of underlying chronic pancreatitis (Case 2). On the other hand, a patient with pancreatic pseudoaneurysm rupture, which was associated with post-operation pancreatitis after pancreatic surgery (PPPD), had a poor prognosis due to a combination of several factors such as surgery, cancer, and old age (Case 4). A comprehensive review of our cases indicated that the prognosis of pseudoaneurysm rupture may be dependent on their underlying causes.
A previous study reported that conservative management of active hemorrhage due to pseudoaneurysm was associated with high mortality, and aggressive and interventional treatment is needed [2]. In the past, surgery was the only treatment for pseudoaneurysm rupture-related pancreatitis with high mortality rates ranging from 10% to 50% [9,10]. However, TAE has been used as one of the less invasive treatment options, with outcomes not inferior to those of surgery. The effectiveness of TAE has been established in handling massive bleeding from gastric and duodenal ulcers, managing visceral artery aneurysms, and dealing with postoperative hemorrhage after abdominal surgeries, with successful hemostasis in 90-92% of cases [11-13]. More recent literature recommends TAE as the preferred treatment method for patients with pancreaticoduodenal artery aneurysms. This recommendation stems from the fact that the anatomical location of these aneurysms, often deeply embedded in the pancreas tissue, complicates surgical ligation, which can result in higher mortality rates compared to TAE [14,15]. Despite the limited number of studies evaluating the efficacy of TAE in treating pancreatitis-related pseudoaneurysms, the reported success rates have ranged from 75 to 100% [3]. In our series, 4 patients were treated with TAE, and 3 of the patients were successfully treated without complications.
In conclusion, pancreatic pseudoaneruysmal rupture is a fatal and potentially life-threatening complication associated with pancreatitis and pancreatic surgery, and TAE could be used for prompt diagnosis and treatment.
Notes
Conflict of Interest
The author has no conflicts to disclose.
ACKNOWLEDGMENTS
Ju Ho Lee helped to refine the tables and figures.

