INTRODUCTION
In 1910, Dr. Purtscher described retinal changes with multiple white spots with scattered hemorrhages in patients with visual loss due to trauma [1,2]. Afterwards, it has been called Purtscher’s-like retinopathy if similar findings were observed in cases other than trauma. The association between Purtscher’s-like retinopathy and acute pancreatitis was described for the first time in 1975 [3,4]. Purtscher’s-like retinopathy is characterized by sudden visual loss after systemic trauma but not by direct ocular injury, and has characteristic fundus findings such as cotton-wool spots, retinal hemorrhage, and papilledema [2].
There are several possible pathogenesis of Purtscher’s-like retinopathy. It is associated with complement activation and may be also developed in a variety conditions such as acute pancreatitis, chronic renal failure, air embolization, and connective tissue diseases [2]. Retinal arteriolar occlusion by complement-mediated leukoembolization is the proposed pathogenic mechanism. Increased activity of proteases such as trypsin, associated with acute pancreatitis might be linked with the production of complement C5a [2,5]. Herein, we report a rare case of Purtscher’s-like retinopathy associated with acute pancreatitis.
CASE
A 28-year-old man with a history of alcohol abuse and no other illness was referred to the hospital because of epigastric pain. He was conscious and hemodynamically stable. He was diagnosed with acute pancreatitis based on clinical symptoms, laboratory findings and computed tomography (CT) findings.
Laboratory blood tests revealed leukocytes 14.1×109/uL, neutrophil 91.8%, hemoglobin 16.0 g/dL, hematocrit 45.0%, mean corpuscular volume 92.4 fl, platelet 201×103/uL, Creactive protein 1.12 mg/dL, total protein 5.8 g/dL, albumin 4.0 g/dL, PT 1.03 INR, aPTT 28.7 seconds, total bilirubin 1.3 mg/dL, direct bilirubin 0.6 mg/dL, blood urea nitrogen 10.3 mg/dL, aspartate aminotransferase 83 IU/L, alanine aminotransferase 139 IU/L, amylase 237 IU/L, lipase 803 IU/L, alkaline phosphatase 87 IU/L, and γ-glutamyltransferase 371 IU/L. Initial abdominal CT scan performed at local hospital was suggestive for acute pancreatitis with CT severity index grade D. One week after hospitalization, the follow up CT was performed and showed mild diffuse swelling of pancreas with peripancreatic infiltration and multiple large fluid collections in peripancreatic area. It was suggestive for moderate acute pancreatitis with Balthazar CT grade E and CT severity index 4 out of 10 points.
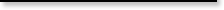
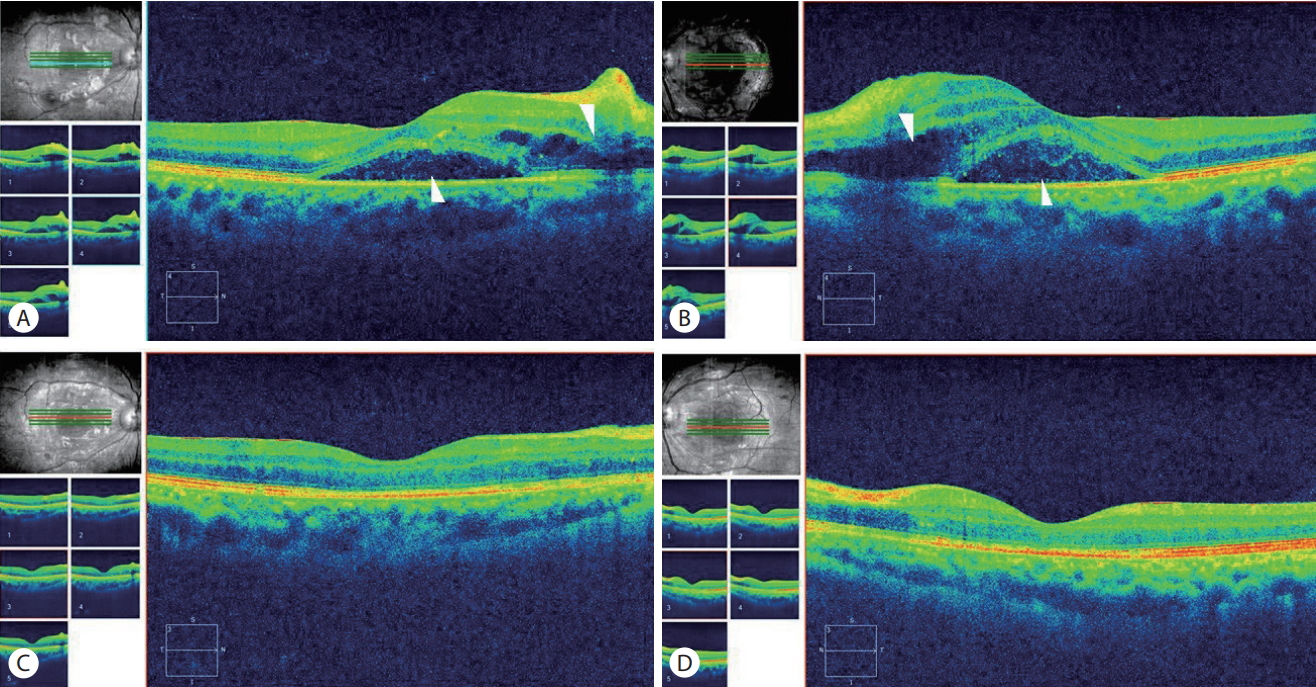
On the second day of hospitalization, he complained of sudden visual disturbance. He had no relevant previous ocular history. Slit-lamp examination and intraocular pressures were normal. Ophthalmoscopic examination of the fundus revealed diffuse retinal whitening (Purtscher flecken) of the posterior pole with confluent cotton-wool spots (Fig. 1; arrows). The arterioles were narrowed, and there were a few superficial hemorrhages (Fig. 1; arrowhead). Optical coherence tomography (OCT) shows macular edema and subretinal detachment in both eyes (Fig. 2A, B; arrowheads). These findings were compatible with Purtscher’s-like retinopathy. After a few days of supportive care, he was recovered from acute pancreatitis.
Two weeks after initial presentation, his vision was significantly improved along with epigastric pain. The follow-up ophthalmoscopic examination showed marked improvement of retinopathy (Fig. 3; arrows). His initial uncorrected visual acuity was 0.8 in the right eye and 0.4 in the left eye. After 6 weeks, his uncorrected visual acuity was improved, being 1.0 in the right eye and 0.8 in the left eye. The macular edema and subretinal detachment also improved on the follow-up OCT (Fig. 2C, D).
DISCUSSION
Purtscher’s-like retinopathy is a rare and severe complication of acute pancreatitis. In Korea, there have been some cases of Purtscher’s retinopathy due to trauma. However, only one case of Purtscher’s-like retinopathy caused by acute pancreatitis after preeclampsia has been reported in 2013 [6]. From what we know, this is the second case of Purtscher’s-like retinopathy associated with acute pancreatitis reported in Korea.
In 1910 Otmar Purtscher described retinal changes with multiple superficial white patches and hemorrhages surrounding the normal optic disc in patients with severe post-traumatic visual impairment [2]. Since then, cases of Purtscher’ s-like retinopathy has been reported in a variety of conditions including childbirth, renal failure, barotrauma, steroid injections in the orbit and nasal passages, infusions of lipidrich suspensions, retrobulbar anaesthesia, cardiopulmonary by-pass, connective tissue diseases and sepsis, all of which may activate the complement system massively [2]. The complement system can cause embolization of clumped granulocytes which can migrate to the retinal circulation and potentially produce the Purtscher flecken via activation of C5a component [5]. In acute pancreatitis, proteolytic enzymes, lipase, kinins, and other active peptides are released from the inflamed pancreas and can cause many complications [3]. These substances can activate the complement system to promote hypercoagulability and this process can change isolated inflammation of the pancreas to a multi-system disorder [3]. The pathogenesis of Purtscher’s-like retinopathy remains controversial, but the most accepted mechanism is leukoembolization that causes arterial occlusion and infarction of the microvascular bed.
Purtscher’s-like retinopathy is diagnosed with characteristic findings of fundus examination. Typically, bilateral diffuse retinal whitening with multiple superficial polygonal patches (Purtscher flecken) are often associated with bleeding, all of which are limited to the posterior pole [5]. There are other possible findings, including venous dilatation, arteriole attenuation, and optic disk swelling [5]. Complement activation is an essential part of the body’s defense, it is likely that Purtscher’s-like retinopathy has occurred more often than actually reported [2]. In 2% of patients with acute pancreatitis, atypical expressions including sudden loss of visual acuity without other clinical causes except alcoholism and chronic liver conditions was shown [7]. There is no correlation between the severity of acute pancreatitis and the presence or absence of retinopathy [4]. The rapid progression of visual impairment is a common and dramatic symptom of this syndrome, although the severity of visual impairment may vary greatly depending on the specific area of retina involved [4]. The visual outcomes of Purtscher’s-like retinopathy with acute pancreatitis vary and are unpredictable [5]. Even if the visual acuity is not fully recovered, the retinal lesion may disappear within 4 months, and the prognosis for visual acuity is unclear [5,7]. If a patient is in a severe condition, she or he may have trouble complaining of symptoms of visual loss. Careful observation of ocular problem should be considered in a patient with acute pancreatitis.
No particular therapy has been proposed other than the treatment of the underlying condition. Some reports have noted improvement of vision after high dose intravenous steroid therapy [5]. It has been noted that large doses of steroid may inhibit both leukoaggregation and free radical-mediated endothelial injury [5]. However, there were many cases in which visual recovery was better in untreated patients than in patients treated with steroids [5]. The efficacy of systemic steroids as a treatment for Purtscher’s-like retinopathy is uncertain. Therefore, clinicians should consider the risks and potential benefits of steroid therapy [5].
The clinical features of our patient were similar to previously reported cases about retinopathy associated with acute pancreatitis. In our case, the retinopathy was full recovered with the clinical improvement of the acute pancreatitis. This rare ocular complication demonstrates the multi-system involvement of acute pancreatitis.