INTRODUCTION
Endoscopic stent placement is a well-established procedure for relieving malignant or benign bile duct stenosis. It has favorable safety profiles. However, there are both early and late onset complications related to endoscopic stent placement. One of the late onset complications is biliary stent migration. This can be either proximal or distal migration. The overall incidence is 3-6% [1].
Proximal stent migration is usually asymptomatic, but it can result in biliary obstruction and cholangitis. In nearly all the cases, proximally migrated stent remains within the biliary tract. The stent migration sticking out of the biliary tract and resulting in hemobilia is very rare. Hence, we report a case of delayed hemobilia caused by penetration of biliary plastic stent into the portal vein.
CASE
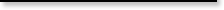
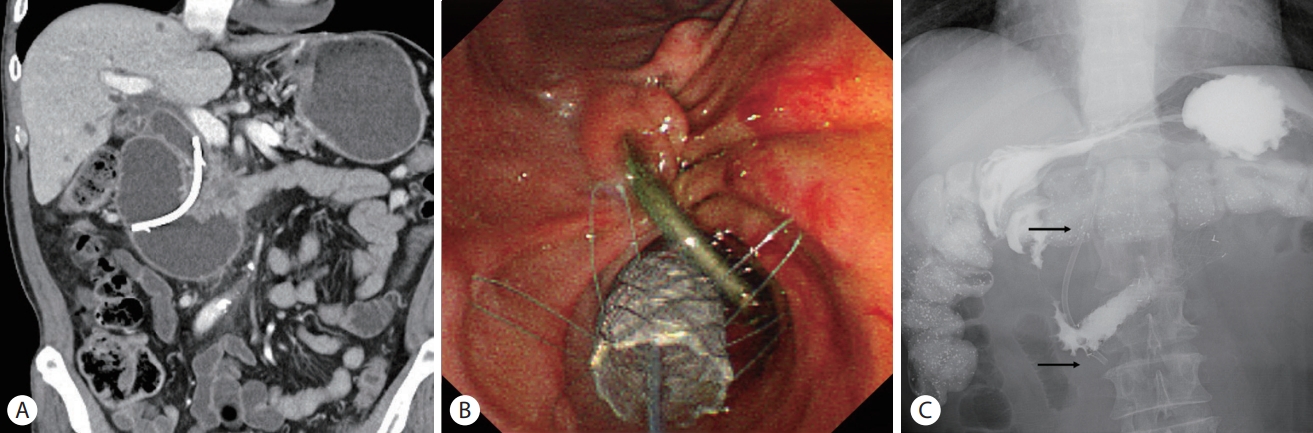
A 66-year-old man was referred to Korea University Guro Hospital for the evaluation of pancreatic head mass. He complained of dyspepsia and sense of abdominal discomfort. Past medical history was remarkable for essential hypertension, diabetes mellitus, and a history of thyroid papillary cancer for which the patient had undergone curative resection 6 months ago. Physical examination was unremarkable. Except for an elevated level of serum carbohydrate antigen 19-9 at 2,384 U/mL, complete blood count and biochemical panel were all within normal range. Abdominal computed tomography (CT) showed a 4-cm sized poorly enhanced mass at pancreatic head and uncinate process with invasion of distal common bile duct (CBD) and duodenal third portion (Fig. 1A).
According to the multidisciplinary discussion, the neoadjuvant chemotherapy was recommended due to invasion of adjacent major vessels. Following endoscopic ultrasonography guided fine needle aspiration confirmed the histologic diagnosis as pancreatic adenocarcinoma. Liver function tests at that time were as follow: aspartate aminotransferase 21 IU/L, alanine aminotransferase 19 IU/L, alkaline phosphatase 74 IU/L, r-glutamyl transpeptidase 63 IU/L, total bilirubin 1.75 mg/dL, direct bilirubin 0.44 mg/dL. Since liver function tests were anticipated to be worsen, endoscopic retrograde cholangiopancreatography (ERCP) was performed and a 10-Fr 7-cm plastic biliary stent (Cotton-Leung ® Biliary Stent; Cook Medical LLC, Bloomington, IN, USA) was placed without immediate complications. The stent was successfully placed across distal CBD stenosis (Fig. 1B, C). The patient was discharged 2 days after the stent placement with no procedure-related complication and scheduled for the next chemotherapy.
Five weeks later with given two cycles of modified fluorouracil, irinotecan, oxaliplatin and leucovorin (FOLFIRINOX) chemotherapy, the patient visited emergency department with vomiting. CT scan of the abdomen demonstrated worsened duodenal invasion of pancreatic head cancer with luminal obstruction at duodenal third portion (Fig. 2A). Initially, a covered metallic stent placement in the duodenum was tried, but distal migration occurred after a week. Then, endoscopic placement of an uncovered metallic stent (HANAROSTENT ® , M.I. Tech, Pyeongtaek, Korea) was done successfully (Fig. 2B, C). After successful duodenal stent placement, the patient was able to resume oral intake and discharged 3 days later.
After 3 weeks from the duodenal stenting, the patient visited emergency department with hematemesis. The blood pressure of him was 92/64 mmHg and pulse rate was 106 beats per minute. The patient’s hemoglobin was 8.7 g/dL, white blood cell count was 14,500×10³/µL and platelet count was 11,800×10³/µL. Liver function tests were as follow: aspartate aminotransferase 39 IU/L, alanine aminotransferase 18 IU/L, alkaline phosphatase 570 IU/L, r-glutamyl transpeptidase 603 IU/L, total bilirubin 2.75 mg/dL, direct bilirubin 1.67 mg/dL. After transfusion of two units of red blood cells, the hemoglobin level was elevated to 11.3 g/dL.
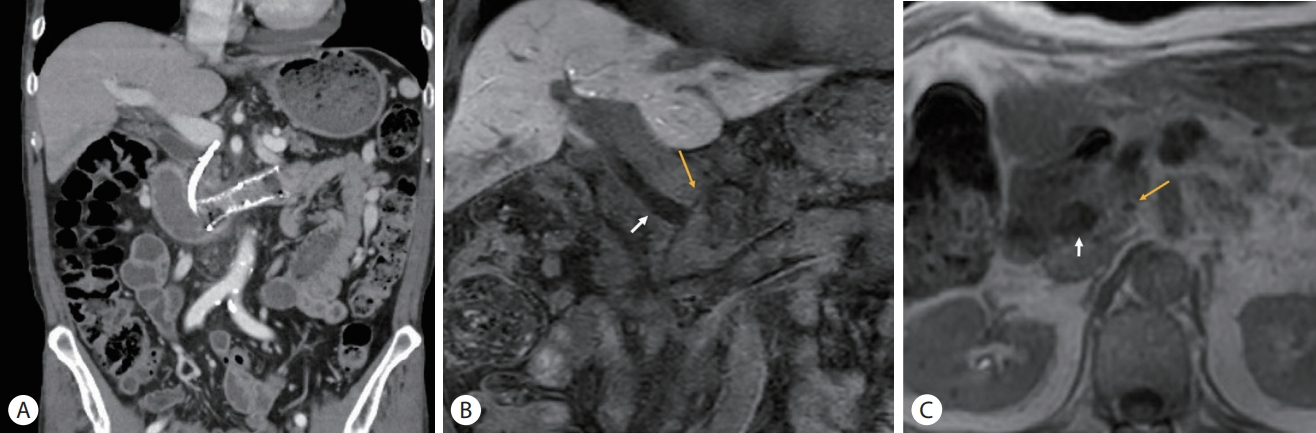
Urgent esophagogastroduodenoscopy (EGD) showed a large amount of fresh blood was found in duodenal second portion. Initially, it was presumed to be tumor bleeding because no causative lesion for active bleeding was found (Fig. 3A). Subsequent angiography demonstrated no contrast extravasation. Magnetic resonance imaging (MRI) revealed a dark signal intensity in the dependent portion of the common bile duct, which was suggestive of blood clots (Fig. 3B). Also, the axis of the previously placed biliary stent was rotated and the proximal tip was headed towards portal vein. In the follow-up EGD, bleeding from the duodenal second portion has ceased, but there was dark blood clot attached to the major duodenal papilla (Fig. 3C). Fortunately, hemobilia stopped spontaneously and did not recur from then.
Follow-up CT scan and MRI were done 2 months later. Previously placed biliary stent has migrated proximally and its proximal tip penetrated into the medial of the CBD and became attached to the portal vein (Fig. 4). We concluded that the migrated biliary stent penetrated CBD and injured the portal vein, which eventually resulted in hemobilia.
Until now, 5 months after from the event of hemobilia, there has been no recurrence. However, despite of eight cycles of modified FOLFIRINOX chemotherapy administered, the overall response is assessed as stable disease. He is treated with the chemotherapy of same regimen as a maintenance.
DISCUSSION
Hemobilia is potentially a fatal condition and often caused by iatrogenic etiology and bile duct invasion of neoplasm [2]. Hepatic artery is the commonly involved vessel with formation of pseudoaneurysm and arterio-bilio fistula. Bile duct communication with portal vein is very rare, and bleeding from such communication tends to be less severe and often self-limited due to its lower blood pressure gradient [2-4].
Percutaneous transhepatic biliary drainage is highly associated with hemobilia, reported as rate of 2.3-3.0% [2,5,6]. However, hemobilia related with endoscopic biliary stenting is rare, and it is mainly caused by direct injury to the bile duct during procedure. Furthermore, it is very rare that endoscopically inserted plastic stent results in late onset hemobilia. There are a few reported cases, indwelling stent made bile duct erosion and formed a fistula with hepatic artery [7-9]. There is another report where a plastic stent penetrates CBD after 5 weeks from ERCP, and it was suggested that weakened and vulnerable bile duct due to cholecystectomy prior to ERCP, has contributed to stent migration and CBD penetration. The migrated stent was surgically removed and primary repair of CBD penetration was performed [10].
In this case, the biliary plastic stent was rotated in opposite direction against to the CBD angulation probably due to traction of endoscope during duodenal metal stenting procedure. Contrary to distal tip of biliary stent fixed by duodenal angulation and metal stent, its proximal tip could stab the angulated portion of CBD by repetitive endoscopic exam in the period of stenting procedure. As a result, the biliary stent penetrated CBD and erode the portal vein with subsequently resulting in hemobilia. It is thought that the bleeding was self-limited owing to low blood pressure of portal vein and stent occlusion with blood clot.
We did not remove the migrated stent promptly when it was found at out of CBD because the recurrence of hemobilia or bile leakage is worried. There was no evidence of biliary obstruction or cholangitis fortunately, even though it would be impending. Delayed procedure is thought to be beneficial for injured tissue to be healed and fibrotic if the patient is tolerable. It could be a favorable option that replacing plastic stent to a large diameter covered stent to overlay the defect of CBD wall.